Do I Have A Trigger Finger? A Deep Dive For Patients Who Want To Know It All
Do you notice a popping, catching, or locking sensation in your finger when you try to make a fist or grab an object? If so, you may have a condition known as ‘trigger finger.’
A trigger finger is a very common hand condition that can cause plenty of pain and frustration. Let’s spend a few moments going over the nuts and bolts of a trigger finger.
My Finger Keeps Popping, Catching, and Locking
As with many entities in hand surgery, in the case of a trigger finger, anatomy explains the findings.
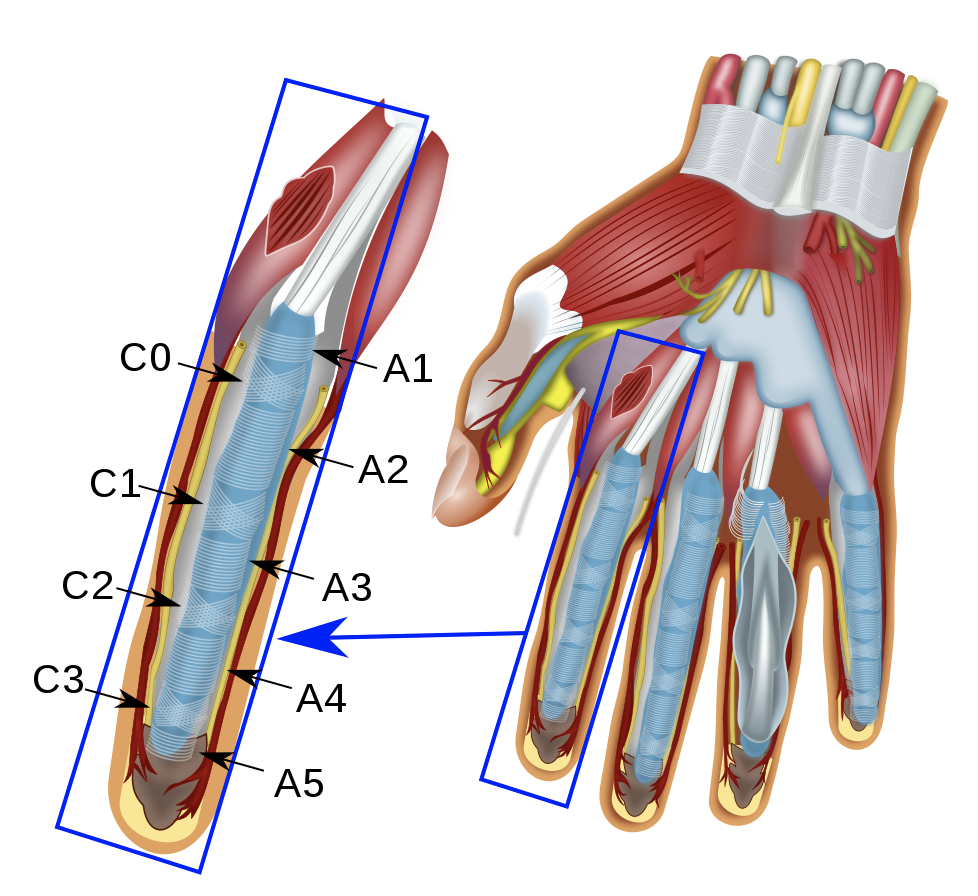
First, curl your fingers into a fist. This action is made possible by long rope-like structures on the palm side of your hand known as flexor tendons (see Figure 2).
When you attempt a fist, your brain activates muscles in your forearm to contract, and these muscles pull on the flexor tendons to bend your finger.
In order to help your tendons function at their strongest, they run through narrow tunnels in the fingers. This tunnel begins in the palm and runs nearly to the tip of each finger.
The tunnel functions as a pulley system to:
Keep your tendon anchored/held down close to the bone, and
Increase your finger’s bending strength (think of a pulley system) and thus your overall grip strength
What is a trigger finger?
How does this anatomy relate to a trigger finger? When you get a trigger finger, your flexor tendon develops a nodule of swelling. Imagine a snake that’s swallowed an egg or a pearl strung on a necklace. In other situations, the sheath (or tunnel) itself can thicken.
The medical term for this phenomenon is stenosing tenosynovitis.
We actually have a low level of understanding about why this occurs. But most of us believe the swelling is the body’s response to a small, otherwise unrecognized injury (as in so many other injuries). Certain conditions such as diabetes, rheumatoid arthritis, or gout can make trigger fingers more likely to occur.
In the majority of cases, we don’t ever get a satisfying answer to why you developed a trigger finger at this one point in time. They do generally increase in frequency as we age.
Now imagine this large ‘egg’ of swelling on your tendon sliding in and out of a tunnel designed for the normal narrow flexor tendon. When you bend your finger down to make a fist, that swollen nodule slips out of the tunnel.
Then, when you try to straighten your finger, that nodule gets pulled back into the tunnel. Or it tries, at least.
Now, the size mismatch between the nodule and tunnel entrance makes this passage difficult, and the result is felt as a *pop* as you bend and straighten your finger. In more severe circumstances, that pop can become painful or your finger may even fully lock in a bent position.
How do I know if I have symptoms of a trigger finger?
The most obvious sign of a trigger finger is…well, a finger that triggers (or catches, locks, or pops)! This can occur in the thumb as well. Other common symptoms can include:
Pain in your palm
A sensation of pain or clicking in the knuckles of your finger or thumb, rather than the palm
Finger stiffness
Worse pain, stiffness, or triggering in the morning
A noticeable tender bump at the base of your finger or thumb
Inability to fully bend or fully straighten your finger or thumb
How is trigger finger treated?
Good news here. Trigger finger is a very treatable condition.
If your symptoms are very mild or appeared recently, there is a reasonable chance they will resolve on their own within a few days to weeks.
Strategies to treat trigger finger at home during this time include over-the-counter anti-inflammatory medications, rest of the affected digit, and gentle stretching.
However, if your trigger finger is very painful, worsening, or not responding to at-home treatment, do not delay in seeing a hand surgeon. Only a hand surgeon can diagnose whether you have a trigger finger versus some other less common cause of finger locking and popping.
Is there a trigger finger treatment without surgery?
Even if you need to see a hand surgeon, this doesn’t mean surgery is your only option. Your doctor can determine if your particular type of trigger finger will respond to a special type of night splint or if it would benefit from a corticosteroid injection.
The majority of trigger fingers can be treated with just one or two steroid injections.
What is the surgery for trigger finger?
In some cases, a trigger finger can become resistant to treatment and would benefit from a small hand surgery.
A surgical release of your trigger finger can be performed under local anesthesia (numbing a small portion of your hand), regional anesthesia (numbing of your whole hand and arm) with ‘twilight sedation’ anesthesia, or general anesthesia (putting you to sleep).
A small 1.5cm incision is made in the palm and a structure called the ‘A1 pulley’ is located.
This A1 pulley is actually the band that makes up the front edge of the tunnel we discussed earlier. This is exactly where the nodule or thickening catches, pops, or locks as your tendon slides in and out of the tunnel.
“The majority of trigger fingers can be treated with just one or two steroid injections.”
This band is released by your surgeon, thus removing the resistance that causes your trigger finger. The rest of the tunnel remains intact, and complications are quite rare following the release of your A1 pulley.
The popping and locking of a trigger finger can be expected to disappear almost immediately after surgery.
Some pain and soreness are expected in the subsequent week or two, but the recovery is generally rapid.
Most patients will regain full finger movement immediately following surgery. The exception to this would be if you had long-standing finger stiffness prior to surgery.
In this case, you may need prolonged hand therapy. In rare cases, chronic finger stiffness before surgery can result in permanent stiffness, even after trigger finger release. Fortunately, this situation is relatively rare.
So there you have it. Now you know a little more about the basics of trigger finger, how it’s diagnosed, and some options for treatment. Hopefully this empowers you to seek the path of care you feel best suited to you and your hand!